Prominent Reports
Implementation Guide (PDF 956 Kb)
Pilot Final Report (PDF 727 Kb)
Artifact Enhancements Based on Pilot Implementation (PDF 406 Kb)
This artifact provides relevant information (i.e. factors) to inform shared decision-making when managing a patient’s chronic pain. The information is presented to the clinician as a Pain Management Summary. The key factors include:
- Pertinent Medical History (Conditions associated with chronic pain and risk factors for opioid-related harm)
- Pain Assessments (responses and scores)
- Historical Treatments (opioid, nonopioid, and adjuvant medications, non-pharmacologic treatments, and stool softeners and laxatives)
- Risk Considerations (morphine milligram equivalent [MME] amount, urine drug screen results, benzodiazepine medications, naloxone or nalmefene medications, and risk assessments relevant to pain management)
Artifact Creation and Usage
This artifact was developed by MITRE software engineers and clinical informaticists, in collaboration with clinical subject matter experts and leaders from the CDC. Additional information about MITRE's health expertise is available here. Additional information about the CDC's response to the opioid overdose epidemic is available here. |
If you would like further information, would like to give us feedback, or have any questions about this artifact, please contact us at ClinicalDecisionSupport@ahrq.hhs.gov
| This CDS logic is expressed using Health Level Seven International (HL7) Clinical Quality Language (CQL) and the HL7 Fast Healthcare Interoperability Resources (FHIR) data model. All value sets referenced in the logic are published on the Value Set Authority Center (VSAC). Additional details about these resources can be accessed via the following URLs: CQL: https://ecqi.healthit.gov/cql FHIRD STU2: https://hl7.org/fhir/DSTU2/index.html FHIR R4: https://hl7.org/fhir/R4/index.html VSAC: https://vsac.nlm.nih.gov/ |
The Pain Management Summary artifact provides relevant information to consider when engaging in shared decision making to manage a patient's pain. The information is presented to the clinician as a Pain Management Summary, implemented as a web-based SMART on FHIR application. The application serves as a CQL integration engine to enable integration of the CQL logic and results with an EHR (such as Epic and Cerner) via the SMART on FHIR API. Implementers should work with their EHR vendor to determine the steps necessary to register and integrate a SMART on FHIR application within their EHR. Technical details regarding the SMART on FHIR API can be found on the SMART Health IT Web site.
The specific method used to invoke the Pain Management Summary CDS and present the SMART on FHIR application is dependent on implementation decisions made at each site. For the initial pilot of this artifact, the site elected to invoke the Pain Management Summary CDS when a clinician clicks on a “Pain Summary Information” link found within each patient record in the EHR.
As discussed previously, the logic used to query and return data for the Pain Management Summary is expressed in the CQL. However, it is important to note that the CQL code does not enact any alerts and/or notifications to reinforce specific CDC guidelines, potential contraindications, or patient safety warnings related to the data that is displayed. Instead, rules were embedded in the SMART on FHIR application to enact notifications displayed as flags, counts, and additional information to further contextual awareness of where a CDC recommendation statement intersects with the displayed data. Future implementers may opt to include the notifications in the CQL; others may opt to expand the notifications in the app. Iterations will likely be informed by capabilities, modules, and the user interface of the EHR, among other considerations.
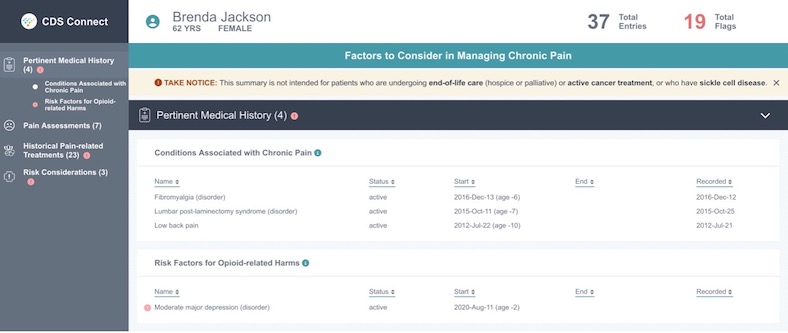
Figure 1 below displays the first portion of a populated Pain Management Summary. The alert flags display as an exclamation point within a red circle to alert the clinician to an entry of potential concern, based on the CDC guidelines. The Summary can be navigated by scrolling or via the navigation shortcuts on the left-hand side of the page.
Figure 1. Pain Management Summary - Header and Pertinent Medical History
The SMART on FHIR application includes logic to flag items of concern for consideration by the clinician. The list of flags in each Summary section are as follows:
- Pertinent Medical History
- Risk factors for opioid-related harms: Always flag if any are present (depression, anxiety, substance use disorder, suicide attempt, sleep-disordered breathing, renal dysfunction, hepatic dysfunction, pregnancy, recent opioid taper, 65 years or older)
- Pain Assessments
- No flags
- Historical Treatments
- Opioid medication: Flag if present
- Nonopioid medication: Flag if NONE
- Non-pharmacologic treatment: Flag if NONE
- Stool softener and laxative: Flag if not present AND at least one opioid medication is present
- Risk Considerations
- If MME is equal to or greater than 50 MME/day
- Urine drug screen: Flag if not present AND at least one opioid medication is present
- Benzodiazepine medication: Flag is present AND at least one opioid medication; Flag if present (each flag has a different message)
- Naloxone or nalmefene medication: Flag is not present AND most recent MME is >=50 MME/day; Flag is present (each flag has a different message)
Additional information provided by the SMART on FHIR application user interface includes the following:
- Counts: Indicates the number of patient clinical entries, as well as flagged entries
- Tooltips: Provide additional information about why the entry was flagged
- Information icons: Provide information on what data was pulled to populate the summary and references
- Uniform Resource Locators (URLs): Provide links to guidelines and additional references.
To ensure accessibility by the widest range of users, the Pain Management Summary application was reviewed by a subject matter expert who addressed all identified issues.
Try the SMART on FHIR app in the SMART App Gallery: https://apps.smarthealthit.org/app/cds-connect
Open source code for the SMART on FHIR app is located on GitHub: https://github.com/AHRQ-CDS/AHRQ-CDS-PAIN-MANAGEMENT-SUMMARY.
Structured code that is interpretable by a computer (includes data elements, value sets, logic)
This CDS artifact presents a variety of key "factors" for clinicians to consider when understanding the history, current circumstances, and therapeutic risks of a patient's chronic pain status and care. This is accomplished by consolidating the factors of a patient's chronic pain by consolidating the factors into a single view, thus easing the burden on clinicians who typically have to navigate to multiple screens and tabs to collect all information needed for a visit. Factors include subjective and objective findings, along with recorded treatments and interventions, to inform shared decision making on treatments moving forward.
This artifact is intended for use in a broad population of patients 18 years or older experiencing a condition associated with chronic pain or receiving a pain medication (i.e., an opioid or nonopioid medication).
Intended for use by clinicians caring for patients 18 years or older in an outpatient setting
Evidence-based source: Although inspired by the 2016 Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain (and reflecting its 2022 update, Clinical Practice Guideline for Prescribing Opioids for Pain), this artifact is not directly derived from any one recommendation statement. Instead, it is meant to complement several recommendation statements within the Guideline by providing a consolidated view of the patient's pain experience and the management of their condition. In particular, the populated pain management summary is intended to promote discussion between the patient and the provider regarding the effectiveness of existing treatments, and the benefits and risks of future interventions while considering the use of nonopioid and/or non-pharmacologic treatment when possible.
Clarification of concept of “adjuvant pain medication” and supporting value sets: In 2022 reviewers clarified the pharmacologic definition of “adjuvant pain medication” to mean “drugs with a primary indication other than pain that have analgesic properties in some painful conditions.” [REF https://pubmed.ncbi.nlm.nih.gov/21254945/] Examples include selected medications for anxiety, depression, or muscle relaxation.
Distinction between CQL logic and the SMART on FHIR app used to integrate and display the CDS: There is a distinction between what is expressed in the logic of this artifact versus the user interface of the SMART on FHIR app that serves as the clinical quality language (CQL) "Integration Engine" for the CDS logic. The CQL logic expresses the inclusion logic and all of the data elements and attributes that populate in the pain management summary. The code within the SMART on FHIR app expresses the logic that supports flagged entries in the summary. The flags are designed to draw the clinician's attention to data of concern, based upon CDC recommendations (e.g., the concurrent presence of an opioid and benzodiazepine medication). Code within the SMART on FHIR app also enables the presentation of tooltip information (e.g., the rationale for a flagged entry).
Exclusion approach: The CDC guidelines exclude patients receiving pain management related to sickle cell disease (added in 2022 guideline), cancer-related pain treatment, palliative care, and end-of-life care. MITRE research identified the lack of availability of patient data representing these concepts in the pilot site's EHR. As a result, an attempt to reason over available structured data would present an incomplete picture of the patient’s health status, potentially leading to inaccuracy of the CDS and a misrepresentation of the patient's health status. After discussion with a CDC representative, the following approach was implemented for these concepts: 1) A notice is presented at the top of the summary for patients who meet the inclusion criteria. The notification reads: “TAKE NOTICE: This summary is not intended for patients who are undergoing end-of-life care (hospice or palliative) or active cancer treatment, or who have sickle cell disease.”. 2) Clinicians were trained on what the CDS logic is able to reason over and where they must use their clinical knowledge and awareness of the patient's health status to make the best decision for the patient. Clinician feedback on this approach is captured in the Pilot Report attached to this artifact.
This artifact intentionally restricts the population to align with the CDC guidelines more closely (e.g., enforces that the patient must be >=18 years old). Future implementers may choose to support a broader population of patients by adjusting the inclusion logic and/or not presenting the exclusion notification at the top of the summary; however they should be aware that changes to the logic may diminish alignment with the CDC guidelines.
Additional information: CDS Connect artifacts are not “standalone” and are not intended to be completely plug-and-play (i.e., healthcare systems will need to integrate each artifact with components of their health information technology (IT) system for the artifact to work). Implementers should conduct extensive testing, including clinical testing in real-life workflows, of all artifacts. It is expected that artifacts will be customized and adapted to local clinical and IT environments.
Although inspired by the 2016 Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain[i], and reflecting its 2022 update Clinical Practice Guideline for Prescribing Opioids for Pain[ii], this artifact is not directly derived from any one recommendation statement. Instead, it is meant to complement several recommendation statements in the CDC guideline by providing a consolidated view of the patient’s pain experience and the management of their condition. Ultimately, the populated pain management summary is intended to promote discussion between the patient and the provider regarding the effectiveness of existing treatments, and the benefits and risks of future interventions while considering the use of nonopioid and/or non-pharmacologic treatment when possible.
For contextual awareness, examples of 2016 CDC recommendations that the summary data indirectly supports include the following:
- Recommendation #3: Before starting, and periodically during opioid therapy, clinicians should discuss with patients known risks and realistic benefits of opioid therapy and patient and clinician responsibilities for managing therapy (recommendation category: A, evidence type: 3).
- Recommendation #8: Before starting, and periodically during continuation of opioid therapy, clinicians should evaluate risk factors for opioid-related harms. Clinicians should incorporate into the management plan strategies to mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (greater than or equal to [≥] 50 morphine milligram equivalents [MME]/day), or concurrent benzodiazepine use, are present (recommendation category: A, evidence type: 4).
- Recommendation #10: When prescribing opioids for chronic pain, clinicians should use urine drug testing before starting opioid therapy and consider urine drug testing at least annually to assess for prescribed medications as well as other controlled prescription drugs and illicit drugs (recommendation category: B, evidence type: 4).
- Recommendation #11: Clinicians should avoid prescribing opioid pain medication and benzodiazepines concurrently whenever possible (recommendation category: A, evidence type: 3).
Note that although terminology and expression of the Recommendations was updated in 2022, all concepts related to the CDS Connect Pain Management Summary are retained in the new guideline.
[i] Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1–49. http://dx.doi.org/10.15585/mmwr.rr6501e1.
[ii] Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. MMWR Recomm Rep 2022;71(No. RR-3):1–95. https://www.cdc.gov/mmwr/volumes/71/rr/rr7103a1.htm.
Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, Recommendations and Reports. (March 18, 2016). CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. 65:1. Retrieved from https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm
CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2022. Retrieved from https://www.cdc.gov/mmwr/volumes/71/rr/rr7103a1.htm
Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2017, Issue 4. Art. No.: CD001431. DOI: 10.1002/14651858.CD001431.pub5 Accessed 16 July, 2024
Shared Decision Making: A Model for Clinical Practice. Elwyn, G., Frosch, D., Thomson, R. et al. J GEN INTERN MED (2012) 27: 1361. https://link.springer.com/article/10.1007%2Fs11606-012-2077-6
Wilcox, A. Jones, S.S., Door, D.A., Cannon, W., Burns, L. Radican, K., Christensen, K. Brunker, C. Larsen, A. Narus, S.P., Thorton, S.N., & Clayton, P.D. (2005). AMIA Annual Symposium Proceedings Archive. Use and Impact of a Computer-Generated Patient Summary Worksheet for Primary Care. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1560720/
Thomas SM, Overhage JM, Warvel J, McDonald C.J. (2001). A Comparison of a Printed Patient Summary Document with its Electronic Equivalent: Early Results. 1067-5027/01 © 2001 AMIA, Inc. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2243457
Lui, Frances, and Kwok-Fu Jacobus Ng. “Adjuvant analgesics in acute pain.” Expert opinion on pharmacotherapy vol. 12,3 (2011): 363-85. doi:10.1517/14656566.2011.521743 https://pubmed.ncbi.nlm.nih.gov/21254945/
Notes outlining the decisions made while interpreting and translating the CDC guideline and while expressing the CDS are listed in the Pain Management Summary Implementation Guide (Appendix A).
- Tigger Type: Named event
- Trigger Event: Provider clicks on link to the Pain Management Summary
Age >=18 years
AND
• Conditions associated with chronic pain (e.g., fibromyalgia, myelopathy, spinal stenosis)
• OR Opioid pain medication
o Orders (within past 180 days)
o Statements (within past 180 days)
• OR Nonopioid pain medication
o Orders (within past 180 days)
o Statements (within past 180 days)
None
| DISPLAY and POPULATE a Pain Management Summary of the following items: | ||
| Pertinent Medical History (unrestricted lookback) • Conditions associated with chronic pain (e.g., fibromyalgia, myelopathy, spinal stenosis) • Risk factors for opioid-related harm o Risk Conditions and Encounter Diagnoses (represented by a union of value sets that define conditions such as depression, anxiety, sleep disordered breathing, etc.) o Pregnancy Diagnosis or Observation in the past 42 weeks o Recent opioid taper o Age >=65 years | ||
| Pain Assessments (lookback of 2 years) • Wong-Baker FACES assessment (score, interpretation, date) • PEG assessment (question response and total score, date) • STarT Back screening tool (total score, date) | ||
| Historical Pain-related Treatments (lookback of 2 years for all except stool softeners, which is 6 months): • Opioid pain medication o Orders (date, active, completed, or stopped) o Statements (date, active, or completed) • Nonopioid pain medication o Orders (date, active, completed, or stopped) o Statements (date, active, or completed) • Adjuvant pain medication o Orders (date, active, completed, or stopped) o Statements (date, active, or completed) • Non-pharmacologic treatment o Orders (date, accepted, in progress, or completed) o Referrals (date) • Stool softener and laxative o Orders (date, active, completed, or stopped) o Statements (date, active, or completed) | ||
Risk Considerations
|
This artifact was tested at a health center affiliated with OCHIN for an 8 week period, from June 20, 2018 - August 20, 2018. AHRQ and MITRE would like to thank OCHIN and their health center member for their partnership on the pilot. The collaborative effort provided a valuable opportunity to test the CQL CDS expression and SMART on FHIR application in a clinical setting and learn from the implementation process and end user experiences.
High-level details are outlined below. Detailed information on the pilot implementation can be found in the Pilot Final Report. Please note this pilot was completed prior to the redefinition and reorganization of the CQL based on a new understanding of the use of adjuvant pain medications as a component of care.
- What went well?
- The CDS was successfully integrated in the pilot site’s EHR and the CQL expression was enhanced because of the pilot implementation.
- The CDS trigger was 100% reliable (i.e., each time a clinician clicked on the link provided in the EHR the Summary was displayed if the patient met the inclusion criteria).
- Clinicians found the CDS “simple and intuitive” to use and the Summary “could be clicked through quickly”.
- Clinicians felt that it reduced burden by removing the need to search through different parts of the EHR for the same information.
- Clinicians felt that the Summary information was beneficial to the care process and informed decision making.
- What did not go well?
- Clinicians experienced a 10 second delay in the display of the Summary. Additional debugging and troubleshooting is required to address this issue.
- The brunt of troubleshooting and debugging fell upon the pilot organization’s technical staff since MITRE did not have permission to access the EHR. Work could have been distributed if MITRE had access to the system.
- Clinicians noted inconsistent display of MME amounts, urine drug screen results and non-pharmacologic treatments.
- The pilot organization rolled out MME calculation in their EHR during pilot kick off and there were still some bugs to be worked out. In retrospect, the MME amount should not have been included in the CDS display until it was fully tested and deemed accurate.
- Inconsistent display of urine drug screen results was not reported until after the pilot ended. Mapping was likely required.
- Due to inconsistent capture and/or unstructured capture of non-pharmacologic treatments during the care process, this concern was expected.
- There were missed opportunities to rectify problems during the pilot (e.g., concerns were not entered in to JIRA)
- What would you do differently?
- Initiate the pilot partnership by March to allow more time for integration and testing efforts, along with pilot site engagement and selection.
- Strive for access to the pilot site’s EHR system, to assist with integration, analysis, troubleshooting and debugging. If this is not feasible, then additional methods to support debugging and performance testing should be explored.
- Engage all individuals in the pilot organization who will be supporting the pilot at the outset of the pilot partnership for situational awareness, collaboration and refinements to the pilot plan.
- What enhancements were suggested by clinicians who used the CDS?
- Integration of the latest Controlled Substance Utilization Review and Evaluation System (CURES) report from the state Prescription Drug Monitoring Program (PDMP).
- Integration of the the patient's pain agreement, including if it was signed and when the renewal date is nearing
- Integration with medMATCH, which indicates if the patient's lab results are consistent with the prescribed medications
- What were the key takeaways/lessons learned from the pilot experience?
- EHRs may not support all FHIR Resources via their API. This should be considered and analyzed as early as possible in the pilot process. Custom development may be required.
- Supporting end users during the pilot is vital. Having a Clinical Champion to maintain end user engagement and raise concerns, an on-site IT resource to serve as a “first line” troubleshooter, and a dynamic feedback system can enhance the success of the pilot.
- CDS integration in an EHR requires a significant amount of planning, time and resources (i.e., a variety of staff members with clinical and technical expertise). The breakdown of time and pilot organization staff resources to achieve CDS integration and implementation this year is as follows:
| Pilot Staff Role/Title | Time spent before the pilot was live (e.g., integration, mapping, testing) | Time spent during the live pilot (e.g., troubleshooting, analysis, reporting) |
| Software Architect (Supervisor/Tech Lead) | 56 hours | 8 hours |
| Quality Assurance Supervisor | 40 hours | 6 hours |
| Medical Informaticist, CDS Lead | 27 hours | 14 hours |
| Business Analyst/Developer (for Reports) | 10 hours | 110 hours |
| Project Manager | 71 hours | 26 hours |



